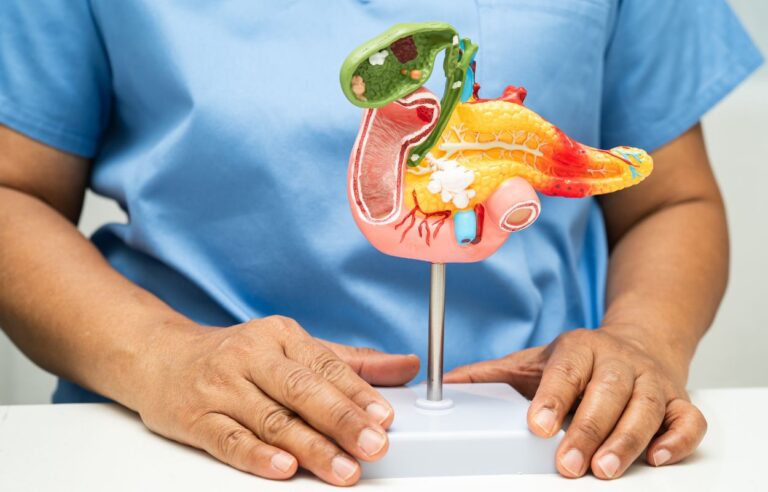
Pancreatic cancer remains one of the most challenging cancers to treat due to its often late diagnosis and aggressive nature. Radiotherapy is a vital treatment modality that uses high-energy radiation to target and destroy cancer cells in the pancreas. This blog post will provide an in-depth overview of radiotherapy for pancreatic cancer, including its indications, advantages, and essential considerations.
Radiotherapy employs high-energy x-rays or particles to kill cancer cells or stop their growth. It is commonly used in pancreatic cancer treatment either alone or more frequently in combination with chemotherapy—a strategy known as chemoradiotherapy. Advances in radiotherapy technology, such as stereotactic body radiotherapy (SBRT) and hypofractionated ablative radiotherapy (HFA-RT), allow for precise delivery of higher radiation doses to tumors, sparing surrounding healthy tissue and minimizing side effects. Typically, radiation is delivered externally using a machine that directs beams to the pancreas with the aid of imaging techniques to target the tumor accurately.
Radiotherapy is used at various stages of pancreatic cancer treatment based on tumor characteristics and patient status:
Adjuvant Therapy: After surgical removal of the tumor, radiotherapy combined with chemotherapy is often administered to reduce the risk of cancer recurrence, particularly in patients with high-risk features such as large tumors or lymph node involvement.
Neoadjuvant Therapy: For borderline resectable tumors (tumors that may be difficult to remove surgically due to proximity to blood vessels), radiotherapy with chemotherapy before surgery can shrink the tumor, thereby increasing the chances of complete surgical removal.
Definitive Treatment: In cases where surgery is not feasible due to locally advanced cancer that has spread beyond the pancreas but not to distant organs, radiotherapy combined with chemotherapy can help control tumor growth and prolong survival.
Palliative Care: Radiotherapy may also be used to relieve symptoms such as pain caused by tumor invasion into nearby tissues, enhancing patient comfort and quality of life.
Local Control: It helps control tumor growth locally within the pancreas and surrounding tissues, which is crucial since many pancreatic cancer deaths are due to local progression.
Pain Relief: Especially in advanced cases, radiotherapy can significantly reduce pain and other symptoms caused by tumor pressure on adjacent nerves and organs.
Shorter Treatment Duration: Techniques like SBRT allow treatment sessions to be completed in about one week compared to several weeks with conventional radiotherapy, which enables patients to resume other therapies sooner.
Potential for Improved Survival: When combined with modern systemic chemotherapy regimens, radiotherapy contributes to improved outcomes, including higher rates of tumor resectability and longer patient survival.
Precision and Safety: Modern radiotherapy uses advanced imaging (such as 4D-CT and cone-beam CT) and motion management techniques to focus radiation precisely on the tumor while minimizing damage to nearby sensitive organs like the stomach, intestines, and liver.
Multidisciplinary Approach: Radiotherapy is most effective when integrated into a comprehensive treatment plan involving surgeons, medical oncologists, and radiation specialists tailoring therapy to each patient’s unique situation.
Side Effects: While generally well-tolerated, radiotherapy can cause fatigue, nausea, and skin irritation. Careful patient monitoring and supportive treatments help minimize these effects.
Ongoing Research: Newer approaches like dose-escalated radiotherapy and combining radiation with innovative systemic therapies are under clinical investigation, aiming to further boost effectiveness and reduce side effects.
In summary, radiotherapy plays a crucial role in the multidisciplinary management of pancreatic cancer. Its ability to control local tumor growth, enhance surgical outcomes, alleviate symptoms, and potentially improve survival makes it an indispensable option. Patients diagnosed with pancreatic cancer should consult specialized cancer centers to explore personalized radiotherapy plans that align with the latest advances and comprehensive care.